The Verily Health Equity Center of Excellence: Addressing demographic disparities in healthcare, by design
As a clinician, population health champion, and federal healthcare leader, I’ve seen firsthand how persistent racial and demographic disparities in healthcare have led to unnecessary suffering and death. In my home state of Louisiana, you can look at a city like New Orleans and see up to a twenty year discrepancy in life expectancy from the predominantly white Garden District to the predominantly black New Orleans East — a community that has in many ways been left behind.
Our mission with the Health Equity Center of Excellence (“HE COE”) is that no community gets left behind. The HE COE is a cross-functional team, building and strengthening our capabilities to reach underserved and underrepresented communities in an effort to afford those communities high-quality, equitable care and research opportunities. We’re embedding principles of health equity and diversity by design into the entire lifecycle of our products, from ideation to development, and post-market processes.
In doing so, I’m hopeful that we can better address these inequities, and address their often tragic consequences. These aren’t just statistics – people’s lives hang in the balance. Verily's core mission is to deliver precision health to everyone, every day. In order to achieve this mission, we need to instill health equity within our products and organization as a foundational capability.
Addressing imbalances in research and care
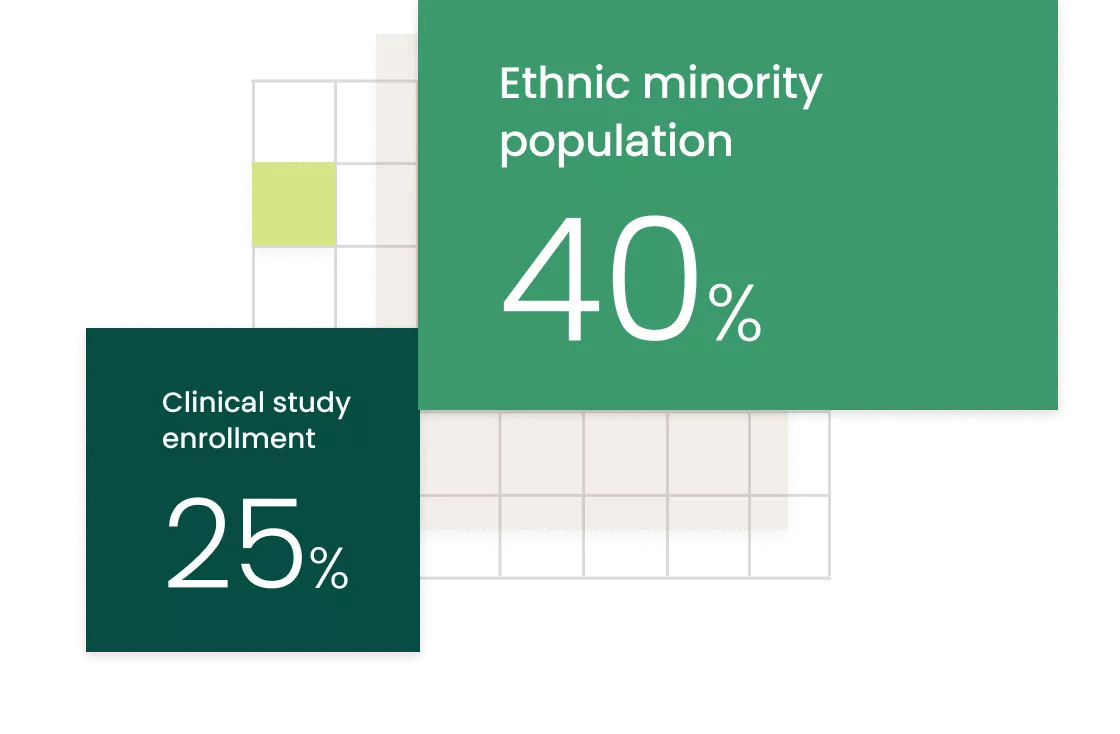
Traditional clinical trials have historically been imbalanced with respect to race, gender and age of participants. Ethnic minorities make up 40% of the population, yet their enrollment in clinical trials that generate evidence for new products is only 25% (FDA). As we stated in a recent publication on DEI in clinical research, the research community has an imperative to make DEI principles key foundational aspects in study conduct in order to pursue better personalized medicine for diverse patient populations. By only studying one group of people, we’re effectively solving for the majority – and hoping it works for the rest of us.
The result? Care and treatment regimes that are blind to the needs of broad swaths of the population. Take, for example, the ubiquitous oxygen saturation monitor. The oxygen saturation monitor does not work as well on Black people, because higher levels of melanin in dark skin can interfere with the light pulses emitted by the monitors measuring blood oxidation. For many years, the accuracy differences by race were considered an acceptable, clinically irrelevant fact of life. That was true for decades until multiple studies showed that these less accurate readings could lead to real differences in care, with possibly negative consequences in outcomes for dark-skinned patients. This example highlights how health equity implications, when not considered early and checked throughout the design and development process, could create harm to historically discriminated and marginalized populations.
We’re already seeing a shift in expectations and action from policymakers: As part of the Food and Drug Omnibus Reform Act enacted in Dec 2022, Congress amended the Food Drug & Cosmetics Act to require clinical trial sponsors to develop “diversity action plans'' for pivotal drug and device studies and submit these plans to the FDA to be considered as part of the formal regulatory package. The requirements for diversity action plans are expected to align with the FDA’s draft guidance on clinical trial diversity once finalized and are likely to encourage sponsors to intentionally develop and justify diverse enrollment targets across race, age, sex and other categories to ensure representativeness in product development research.
Better engagement leads to better data
As technology allows us to expand the data pool with biometrics, wearable devices, and technology that gathers data on the patient experience, collecting and analyzing information is becoming easier and faster. But these data need to be reflective of communities that have been traditionally shut out of the process. If inequitable consequences for underserved and underrepresented populations are monitored only after a product is on the market, we’re reliant on inefficient, reactive, case-by-case corrective actions.
The Verily HE COE will be initially focused on the development of standard practices to ensure diversity, equity and inclusion principles are key foundational aspects in any clinical study with Verily in order to pursue better, personalized medicine for diverse patient populations. We’re using this framework to design studies with our Sponsors that are more inclusive and built with diversity as a key criteria for success. Recently, Verily launched My Skin & Hair Journey, a multi-year study developed with L’Oreal that aims to be the largest and most diverse skin and hair health study. As part of our diversity by design approach, Verily implemented algorithms to optimize digital ads and channels to drive more representative recruitment.
We also launched the Verily Participant Advocacy Panel, our first community co-design group, inviting people with cancer to join to help us design better and more equitable ways to improve treatments across cancer types and fight the disease. Engaging communities in a systematic, structured, longitudinal manner will not only be important for the deep understanding necessary to develop products that are calibrated for health equity, it also begins the path towards generating trust, something that has understandably been eroded. This will take time and a deep understanding of the complexities at play, but it’s something we’re committed to as an organization.
Providing better care and generating better evidence
Another way we’re addressing inequities is to better measure how people actually live their lives. People have a lot on their plate: from work to taking care of family, it can be hard for one to eat healthily and exercise regularly, let alone manage a disease like diabetes which requires consistent attention. Onduo is Verily’s personalized virtual care solution that simplifies and automates the management of type 2 diabetes. By understanding someone’s health and risk factors, tracking glucose levels and other physiological markers, and giving personalized, app-based feedback, Onduo is the nudge that helps patients continue to make healthy decisions when they aren’t at the doctor's office. In fact, type 2 diabetes patients using Verily Onduo saw improvements in both their glucose and cholesterol levels. With a wide range of users, Verily can use aggregated insights, after data use consent, to inform research into new drugs, devices, and treatment approaches that can work for varied demographic groups. This creates a virtuous cycle of care and evidence – patients receive better care, more evidence is generated in the real-world, which can lead to more personalized interventions in the future and ultimately, better outcomes.
Onduo is not the only method through which Verily is leading through diversity by design. The Verily Retinal Service is another solution purpose-built to overcome low healthcare utilization and health inequities by innovating for those who need them most, and by making it easier for providers to improve access to care for more patients. As Verily researchers and engineers worked to design a new, portable camera that supports clinicians in screening for retinal disease, they found that existing solutions had a high rate of unusable, or ungradable, images. Because this discovery was made early in the design process, Verily’s Retinal Service and camera, created a system to successfully image the broadest and most inclusive set of patients possible, by designing for a broad range of variables in physiology. With an overlay of software tools and a focus on primary care settings, Verily is able to enable better access to retinal screenings for anyone selected by their physician for screening.
Health technology brings significant opportunities to expand access to quality research and care. From Verily Onduo’s Spanish speaking capabilities, and access to specialty diabetes care, to our latest partnership with OneOncology and SignalPath, making it possible for community oncology practices to enroll more patients from underrepresented groups.
Putting health equity at the center of what we do
Health equity cuts across all aspects of what we're doing at Verily, as we think about research, care delivery, and integrated devices. By developing standard practices that ensure diversity, equity and inclusion are foundational aspects in our clinical studies and product design, we can create better, personalized medicine for all.