From community to facility: A new frontier in wastewater monitoring
Embracing wastewater monitoring in high-risk settings
Over the last five years, as wastewater monitoring has taken on a critical role in disease surveillance, it has focused largely on data collected from wastewater treatment plants, which represent thousands to millions of users in a geography. This method allows for population-level monitoring of pathogen trends across large communities. However, an emerging use case is monitoring wastewater in facilities to gather information on pathogen circulation in smaller, high-risk communities, like those who live in congregant environments with vulnerable populations, including hospitals and long-term care centers. This approach allows for greater granularity in the information, thereby enhancing infection control, so that more specific interventions can be put in place to address any pathogens of concern.
The case for facility-level wastewater monitoring
During the COVID-19 pandemic, one of the early uses of wastewater monitoring was in buildings on college and university campuses. By January 2021, according to the Covid19 Poops Dashboard1(managed by the University of California, Merced) more than 210 colleges had implemented wastewater monitoring programs on campus.2 The proliferation of these programs was driven by the fact that wastewater monitoring was primarily being implemented by academic researchers, who could easily access these settings. While many of these programs are no longer active, the approach has informed the development of wastewater monitoring programs in other congregant settings, like healthcare facilities.
A notable study3 from researchers Casey Barber and Daniel Gerrity in Nevada highlights the efficacy of localized wastewater monitoring in providing critical insights into the presence of pathogens within targeted populations, such as those in hospitals or care facilities. The study shows how this approach can detect and allow public health officials to respond to outbreaks more swiftly than traditional methods.
In settings like long-term care centers, where staff resources are limited, continuous wastewater monitoring offers a non-invasive, cost-effective strategy to track disease spread. This method is especially valuable for facilities with limited capacity to conduct regular health checks on residents, thereby serving as an "always-on" surveillance system.
Candida auris: An emerging threat and the role of wastewater monitoring
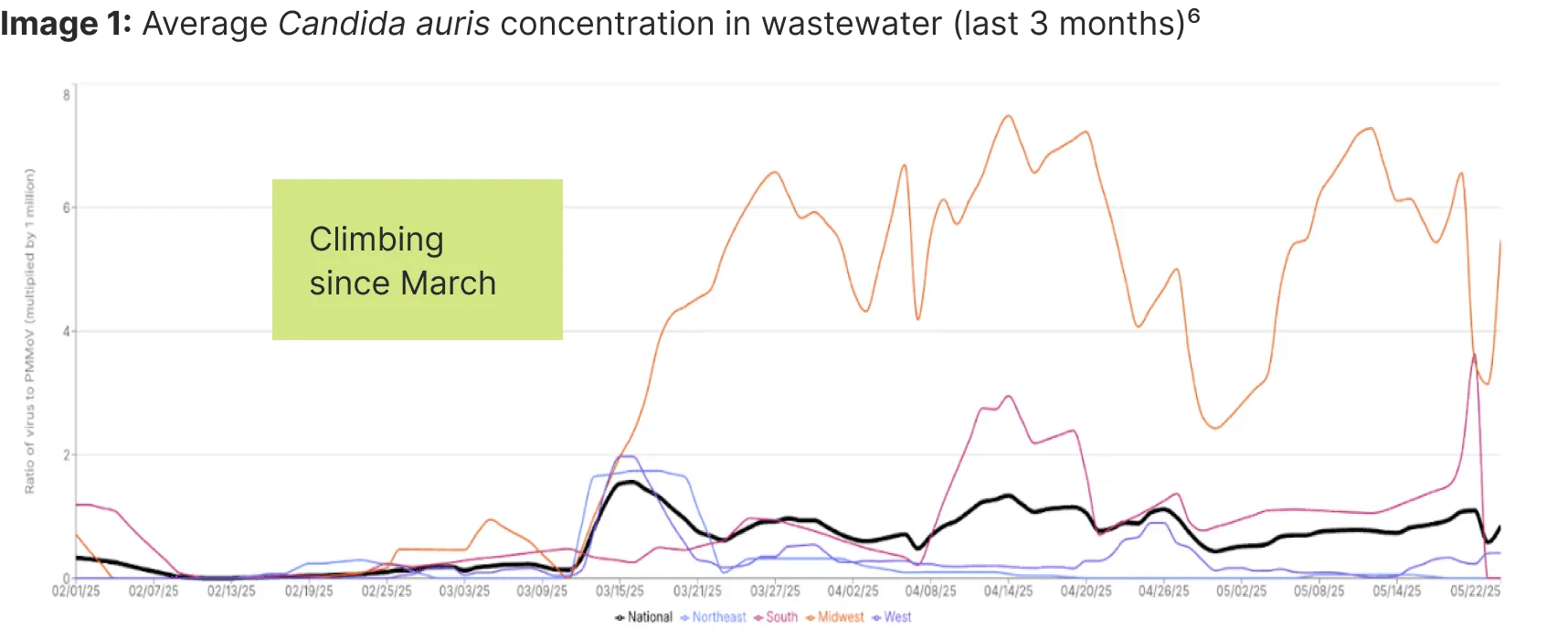
Recently, we have seen a concerning rise⁴ in cases of Candida auris, a drug-resistant fungus, across the Midwestern United States. C. auris is a type of yeast that causes severe illness and spreads among patients in healthcare settings. It can be spread by individuals without symptoms and linger on surfaces, making early identification of risk and infection control challenging. Importantly, most strains of C. auris are resistant to at least one class of antifungal medication, so it is important to limit its spread.⁵
Verily Sightline helps communities prepare for and prevent the spread of infectious diseases
The integration of wastewater monitoring in high-risk settings, like hospitals and long-term care facilities, offers a promising avenue for enhancing public health responses. As we face emerging threats beyond SARS-CoV-2, this method provides a crucial layer of defense, enabling healthcare providers to act swiftly and effectively. By embracing facility-level monitoring, we can better safeguard our most vulnerable populations and stay ahead of potential outbreaks.
Our impact
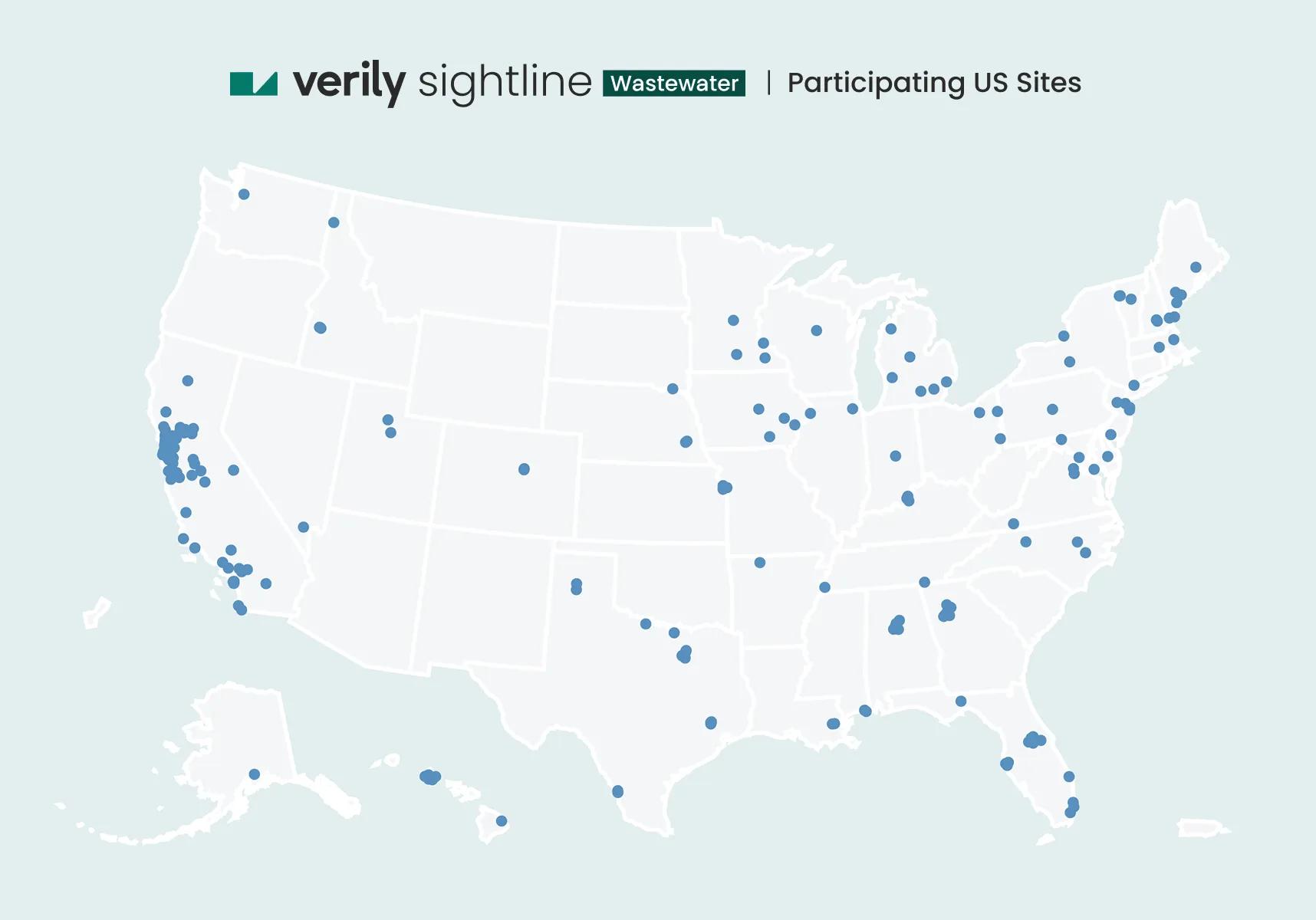
Verily’s wastewater monitoring program provides real-time public health insights and early warning of virus levels in communities, aiding preparation and response to public health issues. See participating sites and learn more at publichealth.verily.com
If you are interested in implementing wastewater monitoring in your community, please contact us here.
Pathogens available for wastewater monitoring:
Respiratory: SARS-CoV-2, RSV A & B, influenza A (IAV), IAV subtypes (H1, H3, H5), influenza B (IBV), human metapneumovirus, human parvovirus B19, parainfluenza (1, 2, 3, 4A, 4B), enterovirus D68, measles
Gastroenteric: Norovirus (GI, GII), adenovirus 40/41, rotavirus
Other: Mpox virus (Clade I, Clade Ib, Clade II), non-variola orthopoxvirus, Candida auris, Hepatitis A, dengue virus (1, 2, 3, 4), Oropouche virus
References
- www.arcgis.com/apps/dashboards/c778145ea5bb4daeb58d31afee389082
- pmc.ncbi.nlm.nih.gov/articles/PMC8122720/
- pubmed.ncbi.nlm.nih.gov/36656763/
- www.nbcchicago.com/news/local/cases-of-drug-resistant-fungus-found-in-17-states-including-illinois/3744564/
- www.cdc.gov/candida-auris/about/index.html
- publichealth.verily.com
- www.cdc.gov/candida-auris/tracking-c-auris/index.html


